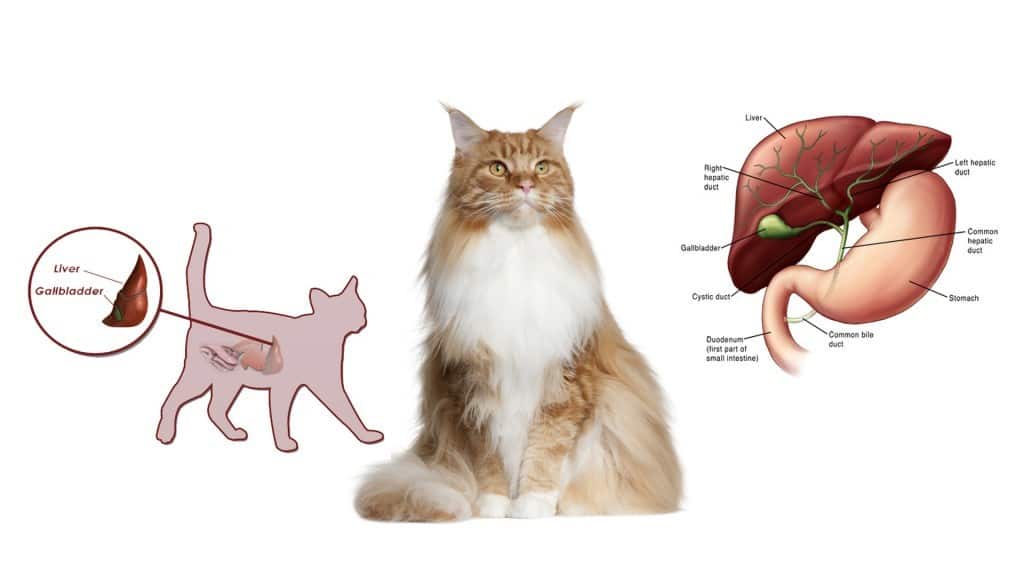
Liver disease in cats can occur in cats of any age, and it occurs when the liver is damaged. The liver is the largest internal organ of the body and is responsible for a number of metabolic, functional and detoxification processes.”¯ It is located in the right side of the abdomen under the diaphragm. The liver is the only organ in the body that is capable of rejuvenating itself.
- Cleanse the blood, removing medications and toxins.
- Regulating chemicals in the blood.
- Produces and secretes bile, which aids digestion and absorption of fats. Bile is a greenish-yellow fluid which consists of bile acids and waste products”¯such as bilirubin. It is made by the liver and stored in the gall bladder.
- Breaks down hemoglogin creating metabolites that are added to bile as pigment (bilirubin).
- Produces specific enzymes which aid digestion of food.
- Converts most sugars into glycerine which it stores up as glycogen until required.
- Fat soluble vitamins A, D, E and K need bile in order to be absorbed by the body; these vitamins are stored in the liver.
- Production of blood clotting factors.
- Manufacture of certain hormones.
- The liver changes ammonia, a toxic by product of protein metabolism into urea, which is excreted in the urine.
The liver”¯is divided into sections (known as lobes), each of which is composed of thousands of structural and functional units (hepatic lobules).
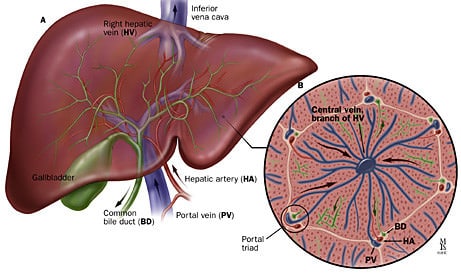
Two blood vessels enter the liver. The hepatic portal vein contains”¯de-oxygenated blood from the spleen, pancreas and digestive system and the hepatic artery contains oxygen-rich blood from the lungs.
Liver Failure
Liver disease in cats occurs when the liver is damaged, resulting in loss of function.”¯It can be acute (sudden onset) or chronic (slow and progressive). The most common cause of liver failure in cats is idiopathic hepatic lipidosis. The next most common cause is Cholangiohepatitis.
Idiopathic Hepatic Lipidosis (also known as Fatty Liver Disease)
Cholangiohepatitis (also known as Cholangitis)
This is a number of related inflammatory and or infectious disorders of the liver and/or the biliary tract. Cholangitis relates to infection or inflammation of the bile duct and Cholangiohepatitis is inflammation of the biliary system and by extension the liver.

Causes of infection may often include feline infectious peritonitis (FIP), Pancreatitis, inflammatory bowel disease (IBD), bacterial infection and parasitic infection (including toxoplasmosis). Feline leukemia and cancers that spread to the liver from other locations are other causes of hepatic insufficiency.
Other Causes of Liver Damage
Toxins
Damage by toxins (Toxic Hepatopathy) is caused by exposure to drugs, toxins or the lack of blood flow to the liver.
Portosystemic Shunt (also known as liver shunt)
Portosystemic shunts are abnormal communications between the portal and systemic venous system which allows intestinal blood to be delivered to the systemic circulation prior to hepatic detoxification. A shunt means that blood bypasses the liver and is not detoxified causing a rise in toxins being delivered throughout the body. Most portosystemic shunts are congenital (known as CPSS) and cats demonstrate clinical signs within 12 months of age.
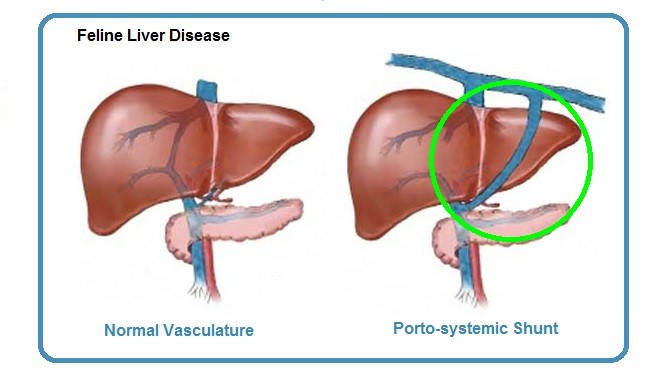
Liver disease can occur in cats of any age although in younger cats it’s most commonly caused by a portosystemic shunt or toxic hepatopathy (ingestion of toxins or drugs).
Symptoms
Clinical signs may vary depending on what has caused the liver disease in cats, and symptoms can often be vague and non-specific.
Early symptoms you may notice include:
- Loss of appetite (anorexia) – One of the early signs of liver disease in cats
- Weight loss – Another early sign of liver disease in cats

- Diarrhea
- Vomiting
- Lethargy
- Bad breath
- Jaundice (icterus):”¯ Signs of jaundice are yellowing of the eyes, skin and mucous membranes. This is caused by hyperbilirubinemia, high levels of bilirubin in the blood. Bilirubin is a yellow bile pigment that is produced by the breakdown of red blood cells
- Ascites (abdominal effusion) – Build-up of fluid in the peritoneal cavity caused by portal hypertension (high blood pressure) in the portal vein of the liver
- Polyuria (increased urination)/polydipsia (increased thirst)
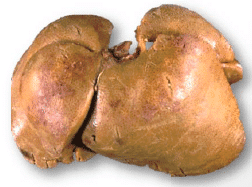
- Hepatomegaly (enlargement of the liver) or micro-hepatica (small liver)
- Dark coloured but clear urine caused by the presence of bilirubin
- Seizures – A build-up of toxins due to the liver no longer functioning properly can lead to seizures
Diagnosis
Your veterinarian will perform a physical examination of your cat and will want to run several tests, including a biochemical profile to look at:
- Changes to the liver enzymes ALT (alanine aminotransferase) and AST (aspartate aminotransferase). The ALT test determines the level of this enzyme in the blood, which increases when damage to the liver cells has occurred. AST is an enzyme also found in skeletal and cardiac muscle cells, the brain and red blood cells. Elevated AST in the blood is also an indicator of liver disease, although as it is found in other organs, it is not as specific for liver cell injury as elevations in ALT.
- Bilirubin: This is a major breakdown product of red blood cells. When red blood cells wear out they are trapped in the spleen and destroyed, releasing bilirubin into the blood. This type of bilirubin is called unconjugated. This bilirubin is transported in the blood to the liver, where it is taken up and conjugated (joined with glucuronic acid). This conjugated form may either be stored in the liver cells or excreted into the bile.”¯ Bilirubin levels are increased in cats with liver disease, gallbladder disease or have excessive destruction of”¯red blood cells (known as haemolysis).
- Low blood urea nitrogen (BUN), albumin, glucose, cholesterol which reflect the liver’s inability to metabolise urea and glucose or produce albumin or cholesterol.
Other tests that may be performed include:
- Complete blood count: May reveal the presence of poikilocytes, which are abnormally shaped red blood cells. Anemia may also be present. Reduced white blood cells or platelets may indicate portal hypertension.
- Urinalysis may reveal ammonium biurite crystals and/or bilirubin in the urine.
- Thyroid testing
- Bile acids tolerance test. This involves taking a blood sample from your cat and then feeding him a fatty meal. Two hours later, a second blood sample is taken. When a cat eats, bile is released into the small intestine to assist with the digestion of fats (lipids). The bile is then absorbed by the intestine and returned back to the liver where it is removed from the bloodstream. In a cat with liver disease, this process doesn’t occur as efficiently and levels of bile remain high in the blood.
- Ultrasound: An ultrasound can give your veterinarian an idea of the size and shape of your cat’s liver and gallbladder, and detect gallstones and biliary obstruction (blockage of the flow of bile from the liver). Abnormal vessels may be seen on ultrasound. Intrahepatic (inside the liver) are easier to see on ultrasound than extrahepatic (outside the liver) vessels.
- X-Ray:”¯ An x-ray may be taken to give your veterinarian an idea of the size and shape of your cat’s liver. X-ray may also detect the presence of tumours.
- Biopsy: A liver biopsy is taken to determine the exact type of liver disease. This may be done at the same time as the ultrasound.
- Serologic Testing: Testing for diseases such as FeLV, FIV, FIP and toxoplasmosis may be taken as these diseases are associated with some liver disorders in cats.
Treatment
Treatment depends on the cause of liver disease in cats.

- Intensive nutritional support. Most frequently this involves feeding a”¯calorie dense, high protein”¯food via a feeding tube either directly into the stomach or esophagus. This type of”¯feeding will usually be required for 6 – 8 weeks.
- Fluid and electrolyte therapy if the cat is dehydrated.
Cholangitis / Cholangiohepatitis complex:
- Supportive care with IV or subcutaneous fluids and nutritional support.
- If the cause is bacterial, antibiotics will be prescribed.
- Medication to control vomiting if necessary.
- Corticosteroids may also be helpful in cats.
Damage by toxins:
- Immediately stopping the toxins (such as medications) where possible.
- Removal of toxins from the body with activated charcoal.
- Supportive care.
Portosystemic Shunt:
- Surgical ligation if physically and financially possible.
- A prescription diet which is restricted in protein may be recommended.
- Supportive care, where necessary.
Acute Hepatic Failure in Cats
Hepatic failure, or acute liver failure, is a condition characterized by the sudden loss of 70 percent or more of the liver’s function. This diseased state may be due to sudden, massive, hepatic necrosis (tissue death in the liver).
Symptoms
Primary and secondary hepatobiliary disorders – those dealing with the liver, gallbladder, bile ducts or bile – are generally associated with variable hepatic necrosis. However, acute liver failure from severe hepatic necrosis is an uncommon phenomenon.
Acute liver failure can affect the body through a number of system failures:
- Gastrointestinal: vomiting, diarrhea, blood in the stool (hematochezia)
- Nervous system: hepatic encephalopathy (brain disease related to liver failure)
- Hepatobiliary: the liver plus the gallbladder; jaundice, necrosis (tissue death) of the liver cells and bile duct cells
- Renal: the tubules of the kidney may be injured from toxins/metabolites
- Immune/Lymphatic/Hemic: imbalances in the blood and lymphatic systems, may lead to coagulant (clotting) complication
Causes
Acute liver failure is most often caused by infectious agents or toxins, poor flow of fluids into the liver and surrounding tissues (perfusion), hypoxia (inability to breathe), drugs or chemicals that are destructive to the liver (hepatotoxic), and excess exposure to heat. Necrosis (tissue death) sets in, with loss of liver enzymes and impaired liver function ultimately leading to complete organ failure.
Acute liver failure also occurs due to extensive metabolic disorders in protein synthesis (albumin, transport protein, pro-coagulant and anticoagulant protein factors), and glucose absorption, as well as abnormalities in the metabolic detoxification process. If this condition is not treated promptly, it can result in death.
Diagnosis
Acute liver failure is diagnosed through a full blood workup (hematology), biochemistry analysis, urine analysis, biopsy (the removal and analysis of affected tissue), and ultrasound or radiology imaging.
Hematology/biochemistry/urine analyses will test for:
- Anemia
- Irregularities in thrombocytes (clot promoting blood platelets)
- Abnormally high liver enzyme activity, or liver enzymes spilling out into the bloodstream, signaling liver damage — tests will look for alanine aminotransferase (ALT) and aspartate aminotransferase (AST) enzymes in the bloodstream, as well as an increase in alkaline phosphatase (ALP), and declining levels of aminotransferases (enzymes that cause the chemical change of nitrogen carrying amino)
- Impairment of protein synthesis
- Low blood sugar — particularly dangerous for cats
- Normal to low blood urea nitrogen (BUN) concentration (i.e., nitrogen level in the urine)
- The presence of bilirubin — the red-yellow bile pigment that is a degraded product of the deep red, non-protein pigment in hemoglobin (the oxygen carrying pigment in red blood cells) — in the urine
- The presence of ammonium urate crystals in the urine
- The presence of sugar and granular casts (solid deposits) in the urine, indicating internal tubular injury from drug toxicity
Lab Tests will be used to look for:
- High values of total serum bile acid (TSBA) concentrations, which will indicate liver insufficiency. However, if non-hemolytic (not destructive to blood cells) jaundice has already been confirmed, TSBA findings will lose their significance in relation to acute liver failure
- High plasma ammonia concentration; this, in conjunction with high TSBA concentrations, would be strongly indicative of hepatic insufficiency
- Abnormalities in blood platelets and coagulation (blood clotting) factors
- Tissue necrosis and cell pathology; biopsy (tissue sample) results will confirm or negate zonal involvements, and identify any existent underlying conditions
Imaging tests will look for:
X-rays and ultrasound tests may indicate an enlarged liver, and other hepatic abnormalities, including conditions that may not be directly related to the liver.
Treatment
Hospitalization is vital for treating acute liver failure. Fluids and electrolytes, along with colloid (the gelatinous substance necessary for proper thyroid functioning) replacements and oxygen supplementation, are key aspects of treatment and care. Your cat will be placed on restricted activity in order to give the liver an opportunity to regenerate. Catheter feeding is recommended for highly unstable patients, while enteric feeding (feeding directly into the intestines) in small amounts is recommended for otherwise stable patients. A normal protein diet with supplemental vitamins E and K is advised.
The common medications used for liver failure are anti-emetics, drugs for hepatic encephalopathy (brain disease, with or without edema), hepatoprotectants (to decrease the activity of aminotransferases), coagulopathy drugs, and antioxidants.

This material is provided for educational purposes only and is not intended to diagnose or treat any disease or condition. All specific treatment decisions must be made by you and your local, attending veterinarian.







0 Comments